Financial Navigator for Advanced Care
Job Summary:
The Patient Financial Navigator is responsible for providing support and advocacy to patients related to the financial impact of their clinical care. The navigator will work with the patients and their families to optimize available options for insurance coverage and address insurance gaps via alternative sources. The Navigator evaluates medical benefits including benefits for pharmaceuticals to identify opportunities to access financial resources to support all phases of care most effectively.Serves as a financial resource to the patient, their families and or designees and the care team and provides ongoing financial counseling and education as necessary
Position Responsibilities:
Identifies and effectively communicates financial information to team members, patients, and their families with emphasis on identifying any potential patient out-of-pocket liability. Establishes relationships with insurance company, pharmaceutical companies, and other patient aid sources to assists patients to explore options for financial assistance to support health and medical needs. Stays abreast of regulations, making certain that applications are appropriate and complete to ensure that the Hospital, the professional groups, and the patient receive all benefits for which the patient is eligible. Works closely with and communicates consistently with Social Work, Case Management, Nurse Navigators and Billing to provide a cohesive support system to the patient and clinical providers.
Obtains all necessary payor authorizations. Verifies coverage and other medical benefits and acquiring necessary referrals and authorizations for inpatient stays and procedures. Responsible for understanding the clinical treatment plan and needs, verifying insurance, checking benefits, and assisting patients with maximizing insurance benefits. Assists patient with maximizing insurance benefits. As appropriate, provides assistance to facilitate applications for assistance. Actively participates in multidisciplinary meetings regarding financial information and barriers for patient’s care.
Works with patients, their families and team members when possible, to help address insurance coverage gaps via alternative funding options.
Obtains and documents detailed patient insurance benefit information including, but not limited to, surgery, outpatient prescription drugs, follow-up clinic visits, and travel and housing if necessary. Analyzes this information to identify opportunities to optimize coverage or access assistance opportunities.
Facilitates resolution of patient billing issues. Serves as a liaison with the professional fee and hospital billing offices to resolve billing questions and issues. Assists hospital claims department with proper identification of and accounting for global contract cases.
Serve as a subject matter expert providing education and resources to patients and the care team. Proactively identifies opportunities to support financial needs of patients.
Manages cost report documents and provides billing department with allowable services that are allowed for the Organ Acquisition costs, assist with obtaining date required by the finance department for the Medicare cost report, any billing concerns, and processes all bills and sends to accounts receivable and accounts payable.
Position Qualifications Required:
Required Experience:
2-3 years of experience in healthcare or public health setting with a combination of the following: patient finance, insurance benefits, financial assistance programs, public health, social services or other community-based background.
Required Education:
Bachelor’s degree in social work or other related field. Greater than 6 years’ experience as a financial navigator or similar role may be able to be considered in place of bachelor’s degree.
Training / Certification / Licensure:
Bilingual in Spanish preferred
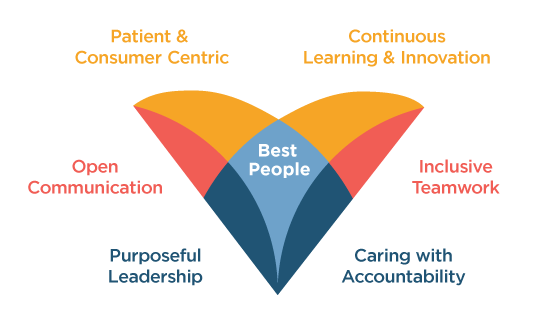
Virtua welcomes all individuals, inclusive of race, sex, sexual orientation, gender identity, religion and faith, national origin, and disabilities, and we proudly look to each person’s unique achievements and experiences to continue to set us apart. Our whole-hearted commitment to an inclusive, diverse, and equitable workplace enables Virtua to be here for our communities, here for our patients, here for our colleagues—Here for Good.
Apply-
Mission:
Virtua helps you be well, get well, and stay well.
-
Vision:
The trusted choice for personalized health care and wellness.
NEWS RELEASES
Read the latest news about Virtua's programs and services, community events, recent awards and more.
See More