Epic Hospital Revenue Integrity Analyst (Hybrid)
- Large hospital or integrated healthcare delivery system experience required!
- EPIC Revenue Integrity, Hospital Billing Certification, HIGHLY preferred.
- Hospital Charge Description Master and charge experience highly preferred.
Job Summary:
The position is responsible for root cause analytics along with audits to help identify opportunities, issues, and process improvement within the Revenue Cycle. This role supports the revenue cycle workflows, charge capture, workqueue and denial review processes within an Epic based EMR.
This position will help optimize Revenue Cycle by evaluating, validating and trending data for presentation to all levels of the organization. Will support the Virtua Hospitals, Physician Groups and Home Health.
Position Responsibilities:
Perform quantitative and financial analysis along with audits designed to identify opportunities for improvement across the full spectrum of the Revenue Cycle.
Assists in ensuring that the charge master and fee schedules are in accordance with government compliance policies and procedures, as well as third party payor needs. Review, identify, and analyze necessary CPT changes related to quarterly and annual AMA CPT updates and regulatory changes by timelines set. Works with revenue producing departments to ensure the ongoing coordinated consistency of the charge master and fee schedules, including accurate descriptions, coding, additions, deletions, pricing, and any other changes. Conduct analytical reviews determine net revenue effect of proposed charge master and fee schedule changes. Perform internal billing audits to ensure correcting coding/billing regulatory compliance and charge capture accuracy.
Incumbent must develop close working relationships with management and staff in Revenue Integrity, Finance, Information Technology and Revenue and Clinical Operations allowing them to perform deep-dive analysis and reviews assisting with the identification of trends, solutions and potential corrective action steps. Will work both independently and have a high level of self-directed work efforts as well as be an integral part of the Revenue Integrity Team. Revenue Cycle will include areas from Hospital, Physician and Home Health.
Monitor and assists with review of revenue cycle workqueues in Epic. Perform analysis to identify issues, trending, root cause, and action plan development with workqueue issues.
Assist in strategic pricing process to optimize reimbursement within budget guidelines. Participate in ongoing coordination and resolution of revenue issues as they arise. Assists in troubleshooting and resolving issues related to the patient revenue cycle, and assists in development and recommendations.
Provide guidance and communication and collaborate with Revenue Integrity Team, Clinical Operations and IT to help ensure workqueue rules are accurate and updated based on annual and quarterly coding changes.
Assist with Epic performance reporting, including assisting with Revenue & Usage, Enterprise Charge Reconciliation and Volume Reports. Workqueue and reporting will include areas from Hospital, Physician and Home Health.
Serve as resource to Patient Financial Services staff for reporting problems and denials on individual claims. Assist in researching coding issues, provide guidance and recommend solution to account representative.
Analyze billing errors and denial data to identify root cause of issues. Work with Revenue Integrity Team, Clinical Operations and Patient Financial Services staff to implement corrective actions to ensure compliant charges, prevent future rejections/denials and accurate and reimbursement. Claim issues and denials will include areas from Hospital, Physician and Home Health.
Lead and participate in projects related to Revenue Cycle initiatives. Participate in ongoing coordination and resolution of revenue issues as they arise. Provide input to Director and Manager for annual Revenue Integrity planning process. Assist with additional projects as needed for Hospital, Physician and Home Health.
Position Qualifications Required:
Required Experience:
3 to 5 years experience within a large hospital or integrated healthcare delivery system.
- Ability to work collaboratively across disciplines and business lines.
- Exceptional oral/written communication skills and highly customer-focused.
- Excellent interpersonal and presentation skills.
- Able to communicate with many, various customers.
- Ability to prioritize, plan and execute.
- Excellent critical thinking, analytical skills.
Required Education:
Bachelor Degree, in Accounting, Finance, Healthcare preferred
Training / Certification / Licensure:
EPIC Revenue Integrity, Hospital Billing, Physician Billing Certification, preferred
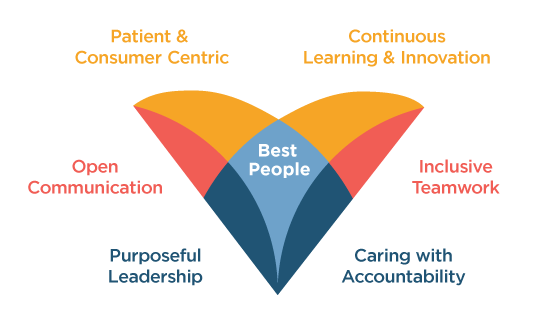
Virtua welcomes all individuals, inclusive of race, sex, sexual orientation, gender identity, religion and faith, national origin, and disabilities, and we proudly look to each person’s unique achievements and experiences to continue to set us apart. Our whole-hearted commitment to an inclusive, diverse, and equitable workplace enables Virtua to be here for our communities, here for our patients, here for our colleagues—Here for Good.
Apply-
Mission:
Virtua helps you be well, get well, and stay well.
-
Vision:
The trusted choice for personalized health care and wellness.
NEWS RELEASES
Read the latest news about Virtua's programs and services, community events, recent awards and more.
See More