Transition Coordinator Per Diem
Job Summary:
Coordinates with referring physicians, care team members, patients and caregivers to provide assistance and resources of services offered within Virtua. Educates and connects consumers interested in Virtua Health to appointments, referrals and utilization of services available across the continuum. Serves as a liaison to coordinate between referring physicians, patients, specialists, and other Virtua services and resources.
Job Responsibilities:
Coordinates resources and services to support transitions in care from the acute to post-acute and ambulatory/community settings.
Facilitates access through follow-up appointment scheduling and resource options to improve patient quality outcomes.
Facilitate acute care transitions to homecare, sub-acute rehab (SAR), acute rehab, and long-term acute care hospital (LTACH) and work with customers to schedule primary care, specialty care and diagnostic testing appointments for transitions in the community.
Coordinate DME (Durable Medical Equipment) providers and transportation services to ensure proper ordering and receipt of DME and assistance in transportation to and from physician appointments where necessary.
The Care Transition Coordinator will work with the divisional Case Management team obtaining post-acute insurance authorizations.
Document all patient interactions in the notes section of EPIC as appropriate.
Perform data entry and complete all data records with concise patient information and appropriate coding to ensure proper tracking of metrics.
Understanding of all databases used such as Epic, Calibrio, CRM, Cisco phone system and Physician database.
Delivers monthly reporting demonstrating outcomes, performance and productivity of service.
Follow-up with patients via telephone and/or correspondences and collaborates with providers as necessary. Maintains confidential records and files/screens telephone calls and resolves routine inquiries/problems.
Develop a thorough understanding of the tests, preps and procedures for the proper and timely scheduling of all Virtua’s clinical services. Have knowledge or understanding of insurance plans, medical terminology and financial assistance programs.
Responsible for outreach efforts to establish and maintain positive working relationships with key customers (physicians, office staff, nurses, etc.)
Participation in quality
Position Qualifications Required:
Required Experience
A minimum of 2-3 years of customer service or call center experience required.
Pleasant and professional communication skills with good diction, tone, and pace.
Ability to work quickly while making accurate decisions is required.
Must be able to use general office equipment including multi-line telephone system.
Proficient in Microsoft Word, Excel, and PowerPoint.
Proficient in the use of Qliq-Connect and Qliqview dashboards.
Required Education
High school degree or equivalent, associate's degree preferred.
Training / Certification / Licensure:
Health care experience including medical terminology and managed care strongly preferred.
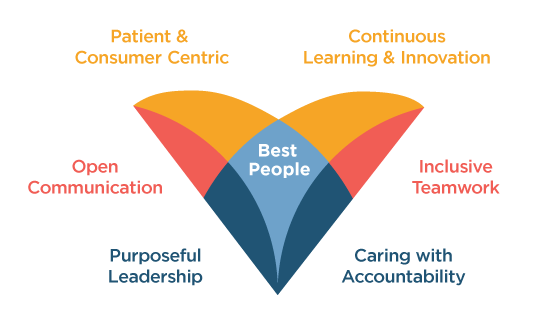
Virtua welcomes all individuals, inclusive of race, sex, sexual orientation, gender identity, religion and faith, national origin, and disabilities, and we proudly look to each person’s unique achievements and experiences to continue to set us apart. Our whole-hearted commitment to an inclusive, diverse, and equitable workplace enables Virtua to be here for our communities, here for our patients, here for our colleagues—Here for Good.
Apply-
Mission:
Virtua helps you be well, get well, and stay well.
-
Vision:
The trusted choice for personalized health care and wellness.
NEWS RELEASES
Read the latest news about Virtua's programs and services, community events, recent awards and more.
See More